Podcast: Play in new window | Download (Duration: 55:42 — 51.0MB)
Subscribe: Spotify | RSS | More
COVID stressed healthcare but showed us a better future.
TL;DR
- COVID revealed what’s broken in healthcare, and also offers a glimpse of how it can be fixed
- Distributed, decentralized and digital isn’t about technology, but about putting patients at the center of healthcare.
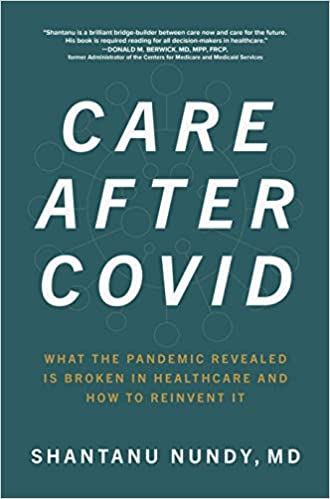
- Read Dr. Nundy’s book Care After Covid: What the Pandemic Revealed Is Broken in Healthcare and How to Reinvent It.
This episode is sponsored by Panacea Financial, Member FDIC. Panacea is banking for physicians and medical students!
Shantanu Nundy, MD, is no stranger to healthcare policy and patient care. He’s a physician, entrepreneur and technologist “passionate about reinventing healthcare for all.” He’s a CMO for a company working to improve health outcomes, a primary care doc in the Washington, DC area, and a lecturer in health policy at the George Washington Milken Institute for Public Health and advisor to the World Bank Group on digital health and innovation.
So we were grateful that he offered to sit down with Dave, M4 Holly Conger, M1s AJ Chowdhury and Rick Gardner, and M3 Emma Barr to talk about his new book Care After COVID. He shows us a future that COVID has revealed as possible for healthcare if we have the will to make it happen: in which technology is a tool that puts patients at the center of everything physicians and systems do.
We Want to Hear From You
How’d we do on this week’s show? Did we miss anything in our conversation? Did we anger you? Did we make you smile? Call us at 347-SHORTCT anytime or email theshortcoats@gmail.com. It’s always a pleasure to hear from you!
What an AI thinks we said360 Care After COVID
Dave Etler: [00:00:00] Welcome Back to the short coat, a podcast of the university of Iowa, Carver college of medicine. I’m Dave Etler. That’s not important right now with me in the studio recording and being live stream to our Facebook group. The Short Coat Student Lounge, which you should join is the incomparable AJ Chowdhury over here is the unparalleled Emma bar.
[00:00:55] The transcendent Holly Congar is over here and in a class of his own it’s Rick Gardner what’s up homies. But if you were thinking that that was all shortcodes well, that’s where you’d be wrong. Joining us today is Dr. Shantanu. a primary care physician technologist business leader. He’s got a new book.
[00:01:15] Care after COVID what the pandemic revealed is broken in healthcare and how to reinvent it out. This may from McGraw-Hill education. Welcome to the show Dr. Nandi.
[00:01:24] Dr. Nundy: [00:01:24] Thank you. I was, I was waiting to hear what adjective I would get, but maybe I have to burn it.
[00:01:29] Dave Etler: [00:01:29] Yeah, we just, either we just, we don’t just give these adjectives.
[00:01:33] Dr. Nundy: [00:01:33] You’re going to make me work for it.
[00:01:34]Dave Etler: [00:01:34] Thank you for, thank you so much for hanging out with us today. I really appreciate it.
[00:01:37]Today’s episode is sponsored by panacea financial division of sauna bank member FDIC. Panacea is banking for medical students and doctors. I’ll tell you more about them later in the show.
[00:01:46] So Dr. Nandi we took a look at your book. I think you’re arguing in the book that COVID has given us an opportunity to see a new future for patient care. Can you elaborate both on this vision of decentralized digital and distributed?
[00:02:00] Care and how
[00:02:01] Dr. Nundy: [00:02:01] it might work. There’s a lot to that. So I think that most of us understand that this has been a once in a century pandemic. Right. But I sort of optimistically look at it as a once in a century opportunity to reinvent healthcare. And there’s really two reasons for that.
[00:02:17] Right. One is healthcare chain has changed more in the past year than it has probably at any time in its modern history, right. Like me as a patient doing my first virtual visits, I did virtual physical therapy on my low back. Right. You know what I’m doing with my own patients. And the second reason is because I think it’s really magnified, not just for doctors, not just for patients, but for really every stakeholder in our country for just how deeply broken healthcare is.
[00:02:48] Right. Like, I think I don’t have any conversations anymore where people don’t talk about health equity like that. Wasn’t. Unfortunately the case a couple of years ago. Right. Or we’re talking about mental health or so I just think that it’s because of both the changes that have happened, but also sort of the understanding that is much more widespread that this is really a special moment.
[00:03:07] So that’s really, the core idea is it’s like kind of the classic, let’s not waste this crisis. Like we have this moment now, what are we going to do with it?
[00:03:16] Dave Etler: [00:03:16] So taking these ideas of decentralized digital and distributed one at a time, I guess what is decentralized? What does that mean in your vision?
[00:03:26] Dr. Nundy: [00:03:26] Yeah. So first of all, let me explain sort of why I think these three words matter, right? Cause I think that like, you know, someone once told me words, create worlds, right. That the way we think about things and conceptualize things really shift. Our minds and then shifts our behaviors. Right. So I’ll ask you to maybe let’s start with distributed first.
[00:03:46] That’s the easiest one to sort of grok, which is I’m sure a lot of us have heard like, Oh, carers become virtualized. Care’s become virtualized. Right. But I always ask, like, has it, I mean, yes, I’m seeing patients maybe through video or through phone. But someone still have to stick a Q-tip in their nose to test code.
[00:04:04] Someone had to get blood work. Someone had to take a medicine every single day. And so I think saying that care has been virtualized is a little bit of a misnomer because it hasn’t a component of it has, but overall , it’s just shifted. It shifted out of clinics and hospitals to being distributed into the community and into people’s homes.
[00:04:26] And so that’s what the concept of distributed is. It’s it’s care happens where health happens digitally enabled. Right. So a lot of people talking about well, AI and EMR and all that stuff. And I think to some degree, we think that those are the technologies that are going to change care. But most of us have seen patients know that the EMR doesn’t really change care.
[00:04:45] Right. It’s we went from a paper form to, we scanned it onto a computer that costs us a hundred billion dollars, but it didn’t really change the way we deliver care. So digitally enabled is saying. Really the role of technology and data is to strengthen the relationships between providers and patients, right?
[00:05:02] That you’re digitally enabling that core interaction. And then do these centralized. It’s sort of a counterpoint to the word value based care. Everyone’s saying value based care, value based care population health. But to me, the key is you can’t just, , wake up one day. He said, Hey doctor, guess what?
[00:05:18] You’re now accountable for that patient’s risk. Like you’re going to manage their risks, right. To do that. You need resources and you need authority. And so decentralized. Power has to shift you. Can’t just give doctors the bag and say, well, guess what, you’re stuck with it. Now you have to give them the tools and the resources and the authority, like simple things.
[00:05:37] Like, my nurses aren’t allowed to go to someone’s house and draw their blood and most States in this country. And so if you want to be able to shift care for people, we need to be, we need to get more than just bearing the risks, which is what most of the value-based care is about. So those are what the three, you know , terms are trying to conjure up.
[00:05:54] Dave Etler: [00:05:54] Thanks
[00:05:56]friends. You’ve stunned them.
[00:06:01] Holly Conger: [00:06:01] Oh, well, I just, I think we’re feeling like we’re talking to an expert, so I’m not sure what I have to add to it, but I know like, I’m an enforcer. So I think as someone who’s about to join the workforce, when I think about like telemedicine and all of its opportunities, I think it’s a great chance to improve healthcare in a lot of ways.
[00:06:16] But you know, the feasibility of it is something that worries me. You know, I think there’s a lot of barriers in place systemically and economically and blah, blah, blah, all those things. And so I just wonder if it will actually be able to happen, you know, cause there’s a lot of patients without digital access.
[00:06:32] And is it actually cheaper to hire a massive amount of MTS nurses, paramedics, or whoever to go home, to home, to home because right now, , all the IMTS and things that we have are just doing emergency care. You know, like I can’t imagine the workforce needed, if all of a sudden there’s that big shift you know, is a virtual visit going to be reimbursed the same way for a physician, because if not, that’s quite the motivation not to do it as a physician.
[00:06:55] You know? Like I just am curious about overcoming a lot of the things in the way.
[00:07:00] Dr. Nundy: [00:07:00] Yeah, no, I think all those are salient points. And again, going back to why I prefer the word distributed, right? Because virtual is a part of it that might work really well for me. It might work really well for you, but for other communities that might be a community health worker coming into your house.
[00:07:15] MTS, I think is a really cool idea. Even just going back to house visits. So like actually house visits have gone up dramatically over the past year. Right? Cause people are afraid to go to a clinic and they’re rediscovering the value of that actually. One of the stories that talk about the book that really did shift.
[00:07:33] My thinking was as you get older, you’re an M four. You don’t have to deal with this yet, but as you get old, like me and you got kids running around upstairs I decided to get life insurance. And I actually had to get a physical exam in order to get life insurance. And of course, like most people and non-compliant patients, like I didn’t get one for years.
[00:07:50] So every time I’d fly it, freak out that like something was kids. One of my friends had, you don’t have to like go somewhere to get your blood work and physical exam they’ll actually come to your house. And I said, Oh, okay. So, you know, I finally signed up this nurse, came to my house, you know, and it was an amazing experience, like actually on the table that I’m sitting on right now, how I got my first EKG I’ve ever had.
[00:08:17]She drew my blood work. I got to like pee in a cup, but in my own bathroom. But the experience was really interesting cause I started putting my myself in her shoes. Right. Like, so she’s driving to my neighborhood where she kind of sees all the tricycles in the yard. Right. She’s walking up my sick stairs.
[00:08:33] She walks in and she sees my prize possession on the right, which is my grand piano. And on the left, you know, as you enter my house, you see like the cities that I’ve lived in and like where I’m married, my wife and where I’ve traveled to. And what made me realize is like, wow, like literally walking into my house, she understood more about me than as a PCP.
[00:08:53] I understand about unfortunately, so many of my patients. Right. And, and that was really profound. And this was an insurance exam. Imagine if this was actually about chronic conditions or actually around mental health or things like that. And so. So, yes, I completely agree. I think thinking of of distributed as, as only about virtual, I think is narrow.
[00:09:15]I think virtual is got a lot of potential. And in many respects, actually the virtual we do is actually the opposite of what we should do. So what happens today with virtual is we actually make urgent visits virtual, which is actually not a good idea. Yeah. That’s what
[00:09:28] Dave Etler: [00:09:28] we were talking about.
[00:09:33] Dr. Nundy: [00:09:33] It should be the primary care follow-up visits that are virtual, because you’ve already met me. I’ve already diagnosed you and done an exam and everything. But now I’m just being like, Hey, how’s the blood pressure medicine going and okay. Are you taking it? Oh, you didn’t get it yet. Okay. Let’s like, so anyways, so much to unpack there.
[00:09:49] Holly Conger: [00:09:49] Yeah. I’m going into emergency medicine. So I think that virtual urgent slash emergency care, it’s probably not a good idea, especially because in this litigious society, like nobody wants to say, you’re fine. Don’t go to the ER, don’t go to the urgent care. You know, like in my experience, almost no one gets told that and they get sent in any way.
[00:10:06] And so then you just have to pay for the virtual visit and the actual visit. But I think that there are a lot of times like any clinic that I’ve been to where I don’t actually do much of a physical exam that could have been a virtual visit, you know? So there’s definitely room for
[00:10:18] Dr. Nundy: [00:10:18] it. Yes, totally.
[00:10:21] Totally. Yeah. And then even on the Homebase, like there’s a organization on, if you guys come across some call ready responders, like they, to your point sent EMT to people’s houses, they can do chest x-rays at home. They can do IB fluids at home. They can give medications at home. Right. So it’s. It’s really interesting, you know, asking the question, like, what is the right care setting?
[00:10:39] Like, it’s kind of like, that’s the whole idea of distributed. We have to get sort of location agnostic, you know, on some level, like, I think it’s right now, it’s just, it’s synonymous with a hospital or a clinic. And I don’t know if that always makes sense.
[00:10:53] Dave Etler: [00:10:53] Yeah. And there are organizations, you know, like I know the visiting nurse association we’ll send people to your house for, care.
[00:10:59]I mean, as you say, there are organizations that do this. It’s just that we don’t always think of it. When the time comes. To do this. And maybe even providers , sometimes don’t even, don’t even think of it, or they might not have the wherewithal depending on where they are in the country or, or you know, if they’re rural versus urban practice, I mean, there’s all kinds of factors there, but it’s not unprecedented.
[00:11:19] It’s just perhaps under utilized and under funded, I guess,
[00:11:25] Dr. Nundy: [00:11:25] probably. Yeah.
[00:11:28] Emma Barr: [00:11:28] Kind of wondering if you have what your thoughts are, if you have any specific thoughts on how this kind of distributed health care works with medical education I’m an MP3. So I went through my core year during the pandemic, having a lot of visits, turn into virtual visits and televisits, and I feel like it impacted my education, but I’m wondering kind of how you see that if we’re doing more distributed care, how can medical students be involved in, you know, still get quality education?
[00:11:55] Dr. Nundy: [00:11:55] Yeah, that’s a really good question. And wow. Yeah, I’m sure you and I could talk for awhile about what he saw this year. It , must be fascinating, but yeah, I mean, I think that at least my training which was a couple of years ago, we did a pretty good job teaching people, clinical medicine.
[00:12:13] We didn’t really teach them to practice the medicine, if that makes sense. Right. And so w and what’s interesting is that the places that are really good at teaching you clinical medicine may or may not be the best places to learn the practices.
[00:12:25] Dave Etler: [00:12:25] So maybe you should elaborate on the difference.
[00:12:28] Dr. Nundy: [00:12:28] And by the way, that’s my own nomenclature.
[00:12:30] That’s not, you know,
[00:12:31] Dave Etler: [00:12:31] I mean, yeah, because I’m. Not a doctor. I don’t, I don’t know everything about medicine. We have listeners who are themselves, not yet doctors.
[00:12:38] Dr. Nundy: [00:12:38] So yeah, of course. Yeah. So what I mean by that is clinical medicine is like, you know what in a textbook or something you’re supposed to do.
[00:12:45] Right? So if somebody comes in with chest pain, what are the questions to ask? What are the tests to order? How do you interpret the test? Right? It’s like, The science part of medicine versus the practice of medicine is, you know, how many minutes did you see a patient for that has chest pain? And, you know how do you get them to tell you the truth about whether they’re drinking or not?
[00:13:07] And how do you make sure that you spend enough time with them, but also get your paperwork done and that you get your coding right? And right. Like all those things. That’s what I kind of need. It’s like the, between the difference. And I think what happens on both sides actually in studies show, this is that if you look at practice variation, meaning differences between me and you and other doctors or other nurses, most of those differences, even 20, 30 years out, or a product of where we be trained, which is fascinating.
[00:13:36] So for example, like I’ll use this blood pressure medicine. And my colleagues in my free clinic will order this blood pressure medicine. And if you ask them. Why it’s not because like we read different papers or like we went to different conferences or because like one of us is smarter than the other it’s because I trained there and she trained there and that’s the medicine that they use.
[00:13:56] Right. And so. My point in this is that when it comes to the science and medicine, lots of places do a great job when it comes to the practice of medicine and particularly distributed care, these sort of newer forms of care, traditional academic medical centers. Aren’t like, they’re the best that the science of medicine, but there may not be the best of the practice of medicine, right?
[00:14:17] They have really long patient wait times. And like, you know, they don’t doctors don’t spend it. Like the experience is not that good, but the problem is because of that 30 year overhang, those habits that we learn about how do you build trust, then? How do you listen and how do you document efficiently?
[00:14:32] And where are you even see patients at home or whatever, how soon you follow up all those habits, we’re learning from kind of not the best places. And so, super long sort of responses to your, your comment, but. I think what we need to do is in training is increasingly expose our trainees to those places and do like away rotations at places that do really good telemedicine based care, or do really good home-based care or do really good population based care.
[00:15:03] And that’s going to mean for many people that you have to leave your school or your residency and go to. The real world where there’s truly places at the cutting edge of how to do that the right way.
[00:15:14] Holly Conger: [00:15:14] Yeah. I think depending on your residency program, that is, or is not built in really well. I know for emergency medicine, at least I will have several months where I’m at a private practice, ER, you know, and so I will get to see like the non-academic version and I I’m going to be at like a County hospital.
[00:15:30]And so I’ll get to see that too. And so I think like depending on where you are and what specialty you go into, some of them build that in and some of them don’t, which I think it’s a great thing because how are you supposed to choose? I want to be an academic physician versus I want to be a private practice physician, if you’ve never seen it.
[00:15:45] Did you
[00:15:45] Dave Etler: [00:15:45] make that choice when you were looking for programs
[00:15:48] Holly Conger: [00:15:48] would never have wanted to sign up where you only get one flavor because you know, how do you, how do you know otherwise? And like he mentioned, you know, Where you are really dictates how you practice a lot of the time, I’ve even seen it as just an M four.
[00:16:01]And I think in Korea, one of the most valuable things that started to grow is actually just my like clinical experience, quote unquote, is where you start looking at a patient and determining that sick or not sick. Like you start being like, I’m really concerned about this person picking up on things and getting better at making clinical decisions.
[00:16:17] I wonder if there’s many studies on, if that still goes well, virtually, you know, like, are you more likely to miss something or is a patient less likely to be honest, virtually or in person? You know, I don’t know. Either one could be better or worse. I just wonder how they compare.
[00:16:32] Dr. Nundy: [00:16:32] Yeah. Yeah. Lots of questions. Yeah. It’s probably
[00:16:35] Holly Conger: [00:16:35] some of you that we don’t have the research yet, but you know, Oh, it’s interesting. Cause it’s like, wow. If my patient is like three times less likely to tell me that they’re feeling suicidal, Via telemedicine, then I’m not going to like that. You know, like I don’t want to risk that or, you know, like whatever the thing may be, you know, that would be something to look into.
[00:16:53] Dave Etler: [00:16:53] You spoke about getting a window into people’s lives that you might not otherwise get with with a more distributed definitely valuable model, which is which I would, I guess not assume is the wrong word, but I would wonder if you know, seeing somebody in their home would make them more likely to talk about their world and the things that are really bothering them.
[00:17:12] Dr. Nundy: [00:17:12] And it
[00:17:12] Holly Conger: [00:17:12] might be, you know, they might feel more comfortable in, so maybe it would be even better for certain specialties.
[00:17:16]Dave Etler: [00:17:16] Hard to know at this point, I think it’s funny cause , we’ve had this ability for a long time. And it took COVID to get us to start thinking about these things, which it makes total sense to me because, so we get so stuck in our ways and , you need you need something to shock you out of , your comfort zone.
[00:17:35] And I think that the most fascinating thing that we learned out of COVID is that not only could we change, but we could change really damn quickly when we had to adapting. So I think that’s really interesting. I you know, one of the, one of the most interesting things to me that came out of COVID was our, , influenza like illness clinic that seems to appear.
[00:17:56] Overnight. Yeah. And then our telemedicine treatment where we were treating people at home through visiting nurses and visiting appointments and things like that, and blood and, and, and monitoring of O two SATs and all this kind of stuff, which again, seemed to happen overnight. And which was.
[00:18:16] Probably critical and keeping our hospital from being overrun. So really neat to see that sort of thing happen I wonder if it’ll last, . I hope it will because I think it makes sense in a lot of ways.
[00:18:27] Dr. Nundy: [00:18:27] Definitely. No, that, that is a really important point.
[00:18:30] Not even just on virtual, but it’s like, it’s like the three most important words I learned or the Ben it maybe is yes, we can. It’s someone who has spent my whole career sort of mucking around and trying to change healthcare. And I’m like, wow, that’s complicated. It’s hard. It’ll take time. And it’s like, yes, we can now will we?
[00:18:52] And do it. And, and part of, I think, what policy makers, cause I get a chance to spend time with some policy folks. I was on a couple of presidential campaigns and stuff is a lot of them are looking at us and saying, wait, when we let safety net doctors text their patients, like we didn’t have all these massive privacy violations that doctors practice across state lines.
[00:19:12] Guess what? Like fraud, didn’t just go up through the roof. Right? So I think part of this, I think the reflection which we have to call it out, if we wanted to see happiness to say, when you actually deregulate parts of healthcare, shit, doesn’t blow up. Actually a lot of it gets better and it enables, this is the whole point of decentralized, by the way, it’s this idea that let the front lines decide.
[00:19:34] AJ Chowdhury: [00:19:50] so I worked as a scribe at a community practice when the pandemic first hit. So for a couple of months, all my experiences were. Typing while the doctor was sitting next to me in their office, talking to patients through a webcam.
[00:20:02] Now I was thinking, wow, this will be really, really helpful for getting more and more patients in to the clinic. But what about when you do go from one clinic to another, from one health system to another, and you change EHR, is that decentralization of data de-centralization of systems, will that hinder or help in that regard where you can have records from one patient be available over Epic, but maybe not
[00:20:28] Dr. Nundy: [00:20:28] over-serving yeah.
[00:20:30] Yeah, totally. I mean, first of all, I’m, I’m usurping the term decentralized and decentralized means specific things to specific people. I’m sort of specifically labeling it in a, in a certain way. That’s different than how most people think of it. Right? Cause like, so for example, like I think most people, when they look at COVID, they say, well, the fact that every state can decide who’s eligible for the vaccine, the fact that like.
[00:20:50] You know, testing was done by different local departments of health was like a failure of decentralization. I’m not talking about that decentralization. I mean, I think, but what you’re talking about is really critical, which is as care gets more distributed, even it’s there is a risk and the risk is that it gets more fragmented.
[00:21:07] Right? And that’s true today. Like if I’m a patient, I can go to my primary care doctor. I could go to the hospital. I could go to an urgent care center. I could call up a digital solution. I could even go to Walgreens and Walmart and see a doc, right? Like care’s already been fragmented like that, that cat is out of the bag.
[00:21:25] But as we move to a more decentralized world where now, or distributed world, excuse me, where you can actually have a home visit too. And you could have an ER person in your home giving you IVs fluids, and you can write, maybe go to the barbershop and get your blood pressure medicine. That’s only gonna increase the risk of fragmentation.
[00:21:42] And so sort of under digitally enabled, I talk about this idea of connected, which is that it creates a much, much greater need for connectivity. And I make the point that connectivity is not just the way that most of the industry thinks about it today, which is okay. Let’s connect EHR, which is critical.
[00:21:59] It’s also has to be true that you have to connect. Care teams and processes, right? Because I mean, already today in my EMR, I have more information than I could ever sift through. Right. And so just the fact that I can have access even more information doesn’t mean that when the patient walks in from clinic a to clinic B, that, you know, I’m creating a connected experience, you know, but if that clinic called me, if we had like a little handoff or other things like that, that plus the data connectivity will create that experience.
[00:22:29] Because I talk about in the book, how, like the, the question that patients dread more than any other question in healthcare is what brings you in today? And the reason is right, because they’re like, wait a second. I called your clinic. And I filled out a form in the waiting room. Then I told your medical assistant, then I told your nurse and baby, I even told the doctor who told me to come to you because you’re the specialist.
[00:22:51] And I walked in and the first thing you asked me is. I didn’t. So like, what brings you in today?
[00:22:58] Holly Conger: [00:22:58] Kind of damages trust. Cause a lot of patients look at you, like, why am I supposed to trust you with my care? If you know, I’ve told a hundred people this and somehow you guys still don’t know.
[00:23:07] And sometimes it’s because there’s that, you know, communication breakdown where you actually just don’t know. But sometimes it’s just, everybody wants to ask because sometimes patients stories change or they say it in a different way and they just want to make sure they got it from the horse’s mouth.
[00:23:20] You have a good
[00:23:21] Dave Etler: [00:23:21] reason for this, but the patients don’t know,
[00:23:26] Holly Conger: [00:23:26] but I’ve been a patient too, you know, and that’s super frustrating when it’s like, I’ve told like six people in the last 10 minutes. What I want and what I’m here, why I’m here? Like, why can’t you just like communicate?
[00:23:35] Dave Etler: [00:23:35] This is the thing I always think of, like calling, calling your gas company.
[00:23:39] And then, you know, the first thing they ask you that the phone tree asks you to input your account number, and then you get, and then you talk to the live person. They’re like, okay, tell me your account number.
[00:23:51] Dr. Nundy: [00:23:51] But
[00:23:53] Holly Conger: [00:23:53] I think the frustrating thing about the EMR in general is if it’s not written down in the EMR, like doesn’t exist. And so like, if you get care from multiple places that are not just under the university umbrella or whatever umbrella, it’s like really hard to like get documents and records and everybody on the same page.
[00:24:08]But I don’t know if. We would all move to like, you know, the Epic monopoly and they just take over the world and they’re the only EMR maybe that would fix it. But yeah, but you know
[00:24:17] Dave Etler: [00:24:17] what I mean? It’s 20, 21. Yeah. You know, like data is data. The key is in my fevered non-expert imagination. The key is making it readable from one system to another.
[00:24:29] I mean, we have ways to do this, you know, whether you’re talking about, , XML or , markup languages, whatever, we can do this in computers. It’s just that we are really bad at it right now.
[00:24:40] Holly Conger: [00:24:40] Yeah. Yeah. I think like the EMR overhead is also like kind of killing private practices a lot of the time, which is probably a separate argument, but that overhead is just so massive that like small businesses, quote, unquote, like just make it very hard for them to exist at all, which is a different argument.
[00:24:55] But, you know, it’s just, I don’t know if that would get better if we’re trying to get like small town, primary care physicians to be able to serve a larger reason region because it’s virtual, you know, like how are they going to support, you know, blah, blah, blah. There’s just lots of questions that this whole telemedicine thing.
[00:25:08] Dave Etler: [00:25:08] Well, and I think, I think sometimes of you know, you’re talking about data from the EMR. And then there are all these sort of , newfangled devices that people are able to get now, like for instance, you know, the Apple watch where you’ve got, a device that can read your heart rate, it can get your blood pressure.
[00:25:25] , they’ve even begun to experiment with glucose monitoring all this kind of stuff, and you can log it and you can keep track of it and you can give it to your doctor and all this kind of stuff. And sometimes I read articles that are like, this is it.
[00:25:37] This is a boon to healthcare. And then I think, yeah, but I know doctors, it’s not that they don’t want that. It’s just that the data becomes overwhelming at some point. How do you sift through all that data for each patient? And you know, I can think of ways around this, like machine learning and all that kind of stuff, but.
[00:25:55] IBM is selling Watson. I don’t really know that that has come to its fruition yet
[00:26:00] Dr. Nundy: [00:26:00] either.
[00:26:04] I think I’ll add that it has to, we have to start with the patient and you have to, you have to go to the care model and then the data and the technology has to support it. Right? So like, let me give, like one of the examples that talk about in the book, right? My mom has had type two diabetes for 25 years, right.
[00:26:21] And for 25 years, what does that mean? That means that she goes to the doctor in 10 minutes. He tells her a bunch of stuff and tells her to like eat healthy. And it says, great. Then she goes home and for a week she does a decent job. Maybe he calls her a week later with her lab results. And then it’s radio silence for six months.
[00:26:38] And then she goes in again and does the same thing. And it’s been 25 years of that. And if you think about the connectivity, let’s imagine that, you know, she had access to all that data from her clinic visit on her mobile phone. Awesome. Let’s imagine that her doctor, every time she saw him every six months, He had a synopsis of all her blood sugar readings, but she hadn’t really looked at this month.
[00:27:01] Let’s imagine that when she goes to an endocrinologist, all the data pops up in a second. Well guess what? She would still be struggling with her diabetes because the . Care model of seeing someone every six months and hoping that they’re going to change their behaviors, doesn’t work. Contrast that to what happened to my mom, which is in June, I’m super proud of her.
[00:27:20] She joined a program around diabetes reversal. Where she was given a, a coach that you can interact with 24 seven. She was given a box that showed up in the mail that had a glucometer and in a ketone meter and a bunch of recipes. She was connected to my family’s from India, another Indian patient who lived in Chicago, who had learned a bunch of recipes that work really well with Indian food.
[00:27:44] And she had an endocrinologist through that same program. And within two weeks, she went from 25 units of insulin to 15. And within a month she was off insulin and it’s been six or seven months. My moms. He hasn’t taken a single shot insulin. Wow. That is amazing. And, and by the way hundreds of thousands of patients have done that now and most talk about medical education.
[00:28:08] Most people that graduate from med school don’t know that you can reverse diabetes. But that’s a whole nother conversation, but my point is that that is how we need to think about solving these problems, right? Because otherwise healthcare becomes this sort of very insular world with like, Oh, well, hospitals are going to connect data to make it easier for doctors to do it.
[00:28:25] I’m like, eh, the job of health reform isn’t to make, I’m sorry to say doctors, licensure, hospitals, Izz, or helper, but our job is to help patients. So how is that connectivity going to help the pain? Now it might, but we got to think about an end to end care model that solves their problem, which is my mom.
[00:28:44] Doesn’t like taking insulin. She wants to get the fuck off of it. If you can, what is the care model required to do that? And then how does technology and data scale and enable that is the question. And I think, we only have a finite amount of resources. You know, Joe Biden, they, they have a hundred dollars to spend on healthcare and for every dollar we spend doing something.
[00:29:04] That perpetuates a broken care model is a dollar we’re not spending on building new care models that actually solve problems for patients. And so that, that’s part of the message I’m trying to give is like, yes. AI. Yes. Connected, I guess. Yes, yes, yes, yes. What about what patients need and want?
[00:29:20] Dave Etler: [00:29:20] This is, yeah, I was thinking about, how healthcare, just how the physical plant of healthcare is set up.
[00:29:27] You know, it’s, it’s all about the, the, the convenience for the system, the convenience for the doctors and the nurses and the PAs and all those people to. Have the patient come to the hospital and have the patient , they’re present in that environment. But , it’s definitely not for the patient.
[00:29:44]So I guess that’s kind of a similar idea.
[00:29:47] Dr. Nundy: [00:29:47] I mean, the most classic visceral example is when we help deliver babies, right? You probably all know about this, but , why are women in stirrups and lying on their backs during delivery? The opposite of what you would want to do, which is let gravity do a job delivered babies in Uganda.
[00:30:03] It’s completely different. Yeah, we do that because it’s like better for the doctors back and they can see it. They can sit in their stool and like, right. Just like the
[00:30:13] Dave Etler: [00:30:13] heart rate, the fetal heart rate monitor. Thing which didn’t work out all that well for my wife. I remember but you know, it’s there to collect data and send it to the nurses station.
[00:30:23] All it couldn’t do. It didn’t work. It was just annoying to my wife.
[00:30:30] Holly Conger: [00:30:30] Yeah. There’s some study that those heart rate monitors don’t actually change outcomes at all because yeah. And so like, there’s plenty of that in healthcare, but I think our whole system, like it’s broken because it’s designed to be reactive instead of preventative, which is like the main problem with our system.
[00:30:45] And, you know, I think a lot of it comes back to, you know, funding, the preventative things, cause putting every person on time with type two diabetes on this program, like your grandma would be wonderful. And I think we would make a lot of difference and avoid a lot of like the long-term sequela of untreated diabetes.
[00:31:01]If we could do that, but it’s just like insurance companies tend to only want to pay for like. Procedures and medications and doctor’s visits, you know? So I was just like, I think restructuring that is our biggest barrier. Same with telemedicine is I’d be curious as do we have insurance companies like treated that like a normal visit, you know, like, do they
[00:31:18] Dr. Nundy: [00:31:18] recognize that?
[00:31:19] I mean, they just it’s temporary still, but they did make that change where they are reimbursed for telemedicine that was changed during the pandemic, which has been a huge enabler. I will, I will though half agree with what you said. So it’s absolutely true that we need policy to change. Like there’s no question about that.
[00:31:37] Right. And it’s true that there’s a lot that we can do. As doctors and med students and individuals. Right. I feel like there’s a little bit of a learned helplessness, like good example, you know, the fact that we’re doing drive-through testing. Now we, as my clinic, we could have been doing this for, for years for a lot of things.
[00:31:56] Yeah. I mean, the idea of putting someone during flu season in a crowded waiting room waiting for 30, we could just have someone standing outside spa and people’s no, we could have done that, but we just, we didn’t lead with that. Like I now prescribe my patients, you know free mindfulness, you know, apps that they can get.
[00:32:13]Even my mom’s, example’s an interesting one, because if you look at how much she’s been paying out of pocket, For her insulin and test strips and stuff like that, versus how much she’s spending on this service. It’s actually almost on par. It’s slightly more that she’s paying for this service which obviously for some patients would be a deal breaker, but I think sometimes we’re like, Oh, well, let’s wait for policy to change. It’s like, nah, we can do this. There’s guard rails that limit us, but there is way more we can and should do for our patients.
[00:32:42]Dave Etler: [00:32:42] I’m gonna take a break to talk about our sponsor for this episode, our friends at panacea financial. Panacea financial was founded by two young doctors because they found other banks, business practices and compatible with the physician lifestyle. They were frustrated by other banks high interest rate co-signer requirements, restrictive loan terms flat-out rejections, inconvenient access to customer service.
[00:32:59] So they built banking specifically for doctors and doctors in training . Panacea offers PRN personal loans for medical students with fast decisions and funding in as little as 24 hours. No co-signer required because you’re adults that’s, you know, why do you need a co-signer anymore? And, and with rates less than half of a credit card, they also offer a totally free checking account with all ATM fees reimbursed across the country.
[00:33:22] So you can take them with you. Wherever you go for medical school, into residency and beyond. Best of all, every customer at panacea gets their own private banker. Their private bankers are supported by a live concierge desk service 24 hours a day, seven days a week because they work doctor’s hours, not bankers hours, and they have a nonprofit arm, the panacea financial foundation investing in doctors and training and working to improve the leaky pipeline.
[00:33:46] For underrepresented, ethnic and racial minorities in the medical profession with scholarships and grant programs. Go to panacea financial.com/match to learn more. Panacea financial is a division of sauna bank member FDA. I see. Thank you for your sponsorship
[00:34:13] Dr. Nundy: [00:34:13] Does
[00:34:14] Holly Conger: [00:34:14] insurance cover any of your mom’s program for the diabetes that’s helping? Does it cover
[00:34:18] Dr. Nundy: [00:34:18] anything?
[00:34:19] It is. It is. They are. So what they did, what they did was because through the program, some of the test strips and things come with like her care package every month, they reimbursed that part.
[00:34:31] Holly Conger: [00:34:31] Okay. But they’re not covering the like additional services, like the
[00:34:34] Dr. Nundy: [00:34:34] coaching, but again, compared to the copays that she was, you know, the $25 every time she saw an endocrine, like if you actually add it all up, it’s almost the same amount.
[00:34:44] That she would have paid it slightly more like on the order of 50 more dollars a year. So it’s pretty close. And then you can think over time about like, well, what if this avoided an ER, visit and stuff, which, you know, there was like, you know, another copay for that and stuff like, it may actually be, you know, cost savings for her, but it’s clearly a barrier.
[00:35:03]You know, but, but there’s also room, I think more room than we think patients paid for a lot of stuff out of pocket, a lot,
[00:35:12] Holly Conger: [00:35:12] like one hospitalization for a heart attack or a kidney, something or anything, you know, it would be worth it to the insurance company. Cause that is so expensive versus paying for this life coach for.
[00:35:22] Or this, whatever the name is diabetes for like 10 years. Yeah.
[00:35:30] Rick Gardner: [00:35:30] Like in this model and you were saying, , like with this example, this anecdote of viewer mother and being able to, if we could like mainstream or inform a, the broader medical community of this, maybe we could start getting people on board with this.
[00:35:43] And that’s the shift having that information and people decide, well, if it’s going to be equally costs you know, the cost is going to be the same, but it’s going to be more efficacious. Maybe we start doing this and that’s where it catches on as a paradigm shift. How do you think that would be implemented or.
[00:35:59] What do you think would be the catalyst for that? Because I mean, I agree it, preventative care is always going to be better. And we should be less reactive.
[00:36:07] Dave Etler: [00:36:07] Well, first of all, you got to get all the old physicians to die.
[00:36:11] Dr. Nundy: [00:36:11] I’m sorry. Retired.
[00:36:14] Dave Etler: [00:36:14] No, I’m kidding. But you know, there’s,
[00:36:16] Dr. Nundy: [00:36:16] there’s inertia. Yeah, no, it’s a great, it’s a great question.
[00:36:19] I don’t know if I have a brilliant answer for that, other than like, this is why I wrote this book. Right. Like, I think that, like, like I said, if you ask most of your classmates graduating from med school the day how ask them is diabetes of reversible disease? What percent do you think will say yes.
[00:36:34] Type
[00:36:34] Holly Conger: [00:36:34] one or type two
[00:36:39] Dr. Nundy: [00:36:39] I think your classmates, I’m guessing less than 10% of them will think it is maybe less than five, maybe less than 1%. And so, and, and that, that’s, that’s another thing we don’t talk about. Right? So in healthcare, right? It’s the classic, it takes 17 years for new clinical guidelines to make it a mainstream clinical practice and were doctors like, Oh my God, I can’t believe those other doctors.
[00:36:58] Like, nah, it’s all of us. Right. And, I talk about in the book, \ it’s like 17 years ago, the iPhone didn’t exist and we went to blockbuster to watch movies. And that’s what it’s like when you walk into a healthcare clinic today in 2021, you’re getting 2004 care. So
[00:37:14] AJ Chowdhury: [00:37:14] speaking of inertia I want to ask since you’ve started to really look into how things have changed with virtual care, since the pandemic began.
[00:37:24]So my aunts are radiologists and whenever anyone asks, if AI is going to replace her, she always responds with no, cause you can’t Sue a computer. What has the legislative landscape will look like since tele-health started getting more insurance coverage and now there’s more actual legislative policies in place to support
[00:37:42] Dr. Nundy: [00:37:42] it.
[00:37:42]So is your question more specifically on like, what’s happened with malpractice around it or started? What, what aspect of it are you referring to specifically,
[00:37:49]AJ Chowdhury: [00:37:49] Big picture view of the landscape surrounding policy and virtual care. Is it moving in a direction that’s better for the patient right now?
[00:37:57] Or is it still early in
[00:37:59] Dr. Nundy: [00:37:59] the process? Got it. Got it. Great. Great question. So first let me tell you what the current state is, and I’ll tell you my opinion of it. So the current state is I think there’s broad consensus on sort of both sides of the aisle that con you know, compared to pre pandemic, telemedicine will be reimbursed.
[00:38:15] Going forward at scale. So like no more requirements, like you have to have seen them in person first and then afterward it can be virtual and no, like what only in places that are medically underserved or only for certain spent, like, I think. The broad consensus is that this is, this is a valuable modality to practice medicine.
[00:38:34] There’s some edge cases that they’re going to figure out, but I think that’s kind of the current state and we’re just waiting for all that stuff to get finalized. My opinion though, is that I have a lot of concerns about how exactly we’re going to do that. So for example, one of the debates right now is like, well, audio only telemedicine can get reimbursed just the same as video based and just the same as an in-person visit.
[00:38:58] Like for some of the reasons we discussed earlier on urgent care and like sick, not sick, like that’s, doesn’t make a lot of sense to me. The other thing is that there’s a risk that telemedicine becomes really transactional, right? Where instead of a proper clinic visit where you like get to know them and all that stuff, that was just like, okay, well, what do you have low back pain.
[00:39:15] Okay. Here’s some ibuprofen, right? And unless we put in place the right framework, whether it’s quality measures or value based care or whatever, I think what’s going to happen is you’re going to sort of. Cater to the lowest common denominator and you’re going to have all these clinics and all these private companies and stuff really just, you know, per, you know, provide frankly low quality care over a virtual telemedicine type service.
[00:39:40] And so I, I think to me, that’s the biggest policy risk is that we’re not really using it to re-imagine that care. It’s not really like the, my mom example, it’s like worse than an urgent care type of example becomes like, you know, as like from a reimbursement perspective, it’s gets reimbursed the same as if you spent 30 minutes on a video, really getting to know them and like taking a tour of their house and like building a trusting relationship.
[00:40:06] Each of those are going to get paid equally the same, and so guess what’s going to happen. And so there’s going to be a missed opportunity, I think to not structure the legislation in the right way. You get to what we all want.
[00:40:16] AJ Chowdhury: [00:40:16] It seems like right now there’s mostly bandages being put in order to treat a symptom, but not addressing the actual underlying cause of what is a, essentially a broken healthcare system.
[00:40:29] Dr. Nundy: [00:40:29] Yes. It gets
[00:40:30] Rick Gardner: [00:40:30] broken at both a like a small scale individual personnel, personal based matter as well as the grand scheme of things is also broken fractured from top to bottom. When you were talking to like the words that came to my mind were like healthcare, industrial complex. We’re going to move to this just.
[00:40:46] Like massive rollout of just proficiency with no excellence in the care or no quality.
[00:40:53] Dave Etler: [00:40:53] Yeah. That was one of my concerns as well in thinking about all this, as, you know, the temptation will be just like with the EMR, a desire to make things more efficient, which, and, and more, you know, sort of cost effective, which I’m not sure that those things always result in good health.
[00:41:12] Holly Conger: [00:41:12] I mean, that system is kind of already still in place now, you know, like people are paid based on how many number of patients do you see a day, which is quite the driver for a lot of doctors to see 50 patients in a day, 60 patients in a day. And it’s like, if you divide up the physical time, that means you’re spending almost no time with each patient, you know, and that’s even an in-person visit.
[00:41:31] So that system is already kind of. There. And so I only imagine it being worse. If you could just get away with a five minute phone call, you know so unfortunately I think that’s a problem we already have. And it’s not unique to the telemedicine idea, but it’s interesting to me that the insurance companies in the billing were just so easy to adopt reimbursing the virtual visits, because they’re so strict about, like, if you want to be billed for this level of patient, you need like a 10 point review of systems.
[00:41:59] You need at least five systems on your physical exam, blah, blah, blah. I’m like all that just vanished, which I think is kind of interesting.
[00:42:07] Dave Etler: [00:42:07] Well, like we’ve been saying all along, Suddenly, we surprised ourselves by how many things were not necessarily necessary. Yeah.
[00:42:14] Rick Gardner: [00:42:14] And it’s funny that we could even like, know that and like have that understanding beforehand, but we still don’t want to change because we’re like either that stubborn or just that stuck in the rut.
[00:42:27] Dave Etler: [00:42:27] I don’t think , many people suspected that those things weren’t necessary, but yeah,
[00:42:31] Rick Gardner: [00:42:31] I would use the example just from like a personal anecdote, like being in the hospital and someone who has a history of Marissa and we still have to put on gowns. But they don’t have an active infection.
[00:42:41] That was something that was happened, but because of PPE, shortages and logistics would, that was something that was early on taken out in this, like, okay, now we can go in without gowns. They don’t have an inactive infection. I, I’m not, well-versed in the science. I’ll preface with that, but it’s like, that’s something that I feel like could have been done earlier, but I guess there was a need to, and it’s surprising that we just didn’t do it earlier.
[00:43:00] Like logistically, I mean, cost effectiveness is still there. And money drives a lot of medicine and a lot of just life in general and especially politics, you know?
[00:43:10] Dr. Nundy: [00:43:10] So yeah, a big area we didn’t talk about, which relates exactly to that is, is. I’m also a really big believer that patients should be allowed to do a lot of stuff themselves.
[00:43:18] Right? So like early independent, the whole reason I wrote this book is because early and pandemic, I wrote a piece that people should just be able to test themselves. And it was crazy to see the response to that. Like I was like in rolling stone magazine, like, it was crazy. My wife’s like who the hell?
[00:43:33] Like, but when I talk to policymakers, like I was in USA today, and this was like, mind boggling is one physician said, how can patients test themselves? Because how can they interpret the result? It has to be interpreted by a physician. Who’s known them for many years to interpret a COVID.
[00:43:55] When was the last time you practiced? Like how many of us. No, our patients for many years, like medicine’s become unfortunately for so many people, so transactional. But then like you said, out of necessity, , we are letting patients test themselves now, right? Like, like door dash delivered to your house and CVS, you can have a little cartridge and test yourself, but been doing this for
[00:44:16] Dave Etler: [00:44:16] years with pregnancy tests.
[00:44:17] I mean, it’s
[00:44:18] Dr. Nundy: [00:44:18] exactly like,
[00:44:20] Dave Etler: [00:44:20] but you don’t need a doctor to, I mean, yes, you might need medical guidance, medical guidance,
[00:44:26] Dr. Nundy: [00:44:26] but a hundred percent. So diabetes is a great example. Pregnancy diabetes. If you have diabetes, you can test yourself for your sugar. Right. But you can’t diagnose yourself with diabetes with the same test.
[00:44:39]And that’s like, you know, and so like, again, if somebody is sitting there saying, I want to get screened for diabetes, because I’m just worried about it. It’s a whole rigamarole it’s I have to have insurance. I have to look up who’s available. I have to find a doctor, which by the way in America is about a three week, wait on average, then I got to take a half day, all this stuff just to test themselves for, for whether or not to teach themselves whether or not they have a risk or have diabetes.
[00:45:04] And so it’s, it gets to your point. It’s like, I think it’s, it’s forced us to question things that at least I’ve been questioning for years. And now the question is like, Yeah. Are we going to revert? And then for a bunch of other stuff that doesn’t make sense, that’s not related to COVID. I mean, most healthcare that’s changed.
[00:45:19] The vascular is like acute COVID, upper or viral respiratory stuff, but can we take that same sort of fresh thinking and apply it to all parts of healthcare and say like, do women really need, who’ve been on an oral contraceptive for 10 years, really need a refill from me. Oh my God,
[00:45:40] Dave Etler: [00:45:40] this is the exact thing that I was thinking about was, you know, like I’ve been on this medication for 20 years and yet I still have to you know, get that prescription reauthorized every single year.
[00:45:52] And I have to do it in person with my physician, which I understand part of it is to just get me there so that he can actually do a well person physical but Oh yeah,
[00:46:01] Dr. Nundy: [00:46:01] every year I’m like so many people, like maybe you have a job that allows you to make it, you have held, but imagine for people who can do that.
[00:46:09] And so then we’re like, Oh, they’re not compliant. They fell off their medications. They’re just like, well, they’re alternative. Isn’t just an annoyance. Their alternative is actually no care. Yeah, right. And so again, it’s like, are we going to question these things and are we going to change things? Are we just going to let it all go?
[00:46:25] And that’s, that’s part of what I mean by decentralized is putting power resources and, and, and responsibility onto frontline teams and to patients like patients can do a lot more than we give them credit for.
[00:46:38] Rick Gardner: [00:46:38] I really liked even. So you made a reference to another book you had written and I’m like . Working with my dad to like, try to make sure he’s a healthy individual and you wrote a book and I, I forgive me.
[00:46:47] I can’t remember the name of it. But essentially like here’s a guide for like every, I think it was like decade of life and what you need to do. And I think that education, because I think we’ve talked about previously medical education and health education within America has failed. So people don’t know how to take care of themselves.
[00:47:02] And so having a book like that and, and information of how to take care of yourselves and giving at least power to the patient and the person to make actionable steps towards their own health is,
[00:47:13] Dr. Nundy: [00:47:13] is correct. Yeah. Yeah. And that’s, you know, I want to end on a, on a sort of a positive note, but I think that’s some of the real revolution that’s happened.
[00:47:20] Right? Like I think they think about patients they’ve realized that they can actually prevent the flu, like who they touch, how close they stand. Right. You’ve had, we don’t know the numbers, but I have had countless patients by their first blood pressure cough. Use a pulse oximeter for the first time, right.
[00:47:37] At home, like find where to get vaccines themselves, find where to get tested. They know what a sensitivity and specificity is like. They’re reading about every single day. Now through social, like I think there’s been, you know, we’ve been wanting patients to take more control, but this, this has created a massive cultural shift that I don’t think we fully understand and policies can change, but I think culture shift, like you remembering, , and sort of the impact of you finding your own test, your own vaccine, you know, managing your own refills.
[00:48:09] Like I think that is going to sustain for a long time. And I think it’s going to create enormous opportunities to improve
[00:48:17] Dave Etler: [00:48:17] health care. Yeah. it sort of reminds me of the fact that , the other day I was marveling that I a have not gotten a cold this winter and B despite the fact that I’m not supposed to get a flu shot.
[00:48:29]I haven’t for the first time gotten the flu in a while and you know, all that is because I learned to wear a mask. And, you know, also was home a lot, but I keep thinking, I had like next year, am I going to, am I going to wear a mask? When I ride the bus to work? Am I going to wear a mask? Like you made
[00:48:46] Rick Gardner: [00:48:46] a point in your book that like you compared it to nine 11 in that there is a before and an after, that’s something that I’ve said.
[00:48:54], I think we have faced a point of no return that things just cannot go back to where they are. Like the example with the mask. I think we will see more masks. Our generation of individuals will they’re in like commuting to work using mass transportation, or even out in the restaurants and such a mask will be more visible.
[00:49:11]Which is something that we haven’t seen in America. And I think other things within healthcare politics socio-economics what, may have you I think that’s a huge thing as we have entered into a new era of
[00:49:21] Dr. Nundy: [00:49:21] life. I wonder if the next normal, yeah, totally
[00:49:28] Dave Etler: [00:49:28] speaking of the post COVID era do you have a listener question?
[00:49:31]Justin would like to know. Yeah. Living in a post COVID 19 era, do you believe that there will be bigger push for developing technologies? And his example is , remote, robotic surgery, more prevalent in the healthcare setting. That’s a, that’s like a, that’s like a
[00:49:47] Holly Conger: [00:49:47] big, that’s a big, that’s a big,
[00:49:50] Dr. Nundy: [00:49:50] yeah.
[00:49:51] Yeah. I think absolutely. I mean, I think that as care moves out of facilities into clinics and then into homes and to communities, that’s going to require a whole shift in technologies. Right? Part of it is taking existing technologies and making it actually consumer friendly, right?
[00:50:08] Like if you’ve ever operated like an event or like even trying to figure out how an IV pump works, like once we start delivering that at home and patients are doing it themselves, it’s gonna right now, basically the technologies that are built are like the ones that get the biggest discounts and sort of cost plus pricing.
[00:50:25] It’s going to shift towards ones that are actually functionally useful. And those that’s going to be a whole dimension. And so I think that that is going to take existing technologies to do that. And then I think it’s going to drive a whole bunch of new technologies. Like one of the like backend ones that I think is gonna be huge is how do you manage and to end supply logistics, which is not that sexy, but when you’re in a hospital and someone orders that antibiotics, it’s pretty easy to like, get it up to the floor.
[00:50:50] Imagine if you’re being hospitalized at home, how do you get someone that’s that antibiotic, or if you are getting oxygen at home and suddenly the tank runs out. So how do you manage that? That’s going to require a whole new set of new technologies. I think there’s going to be a lot of delivery technologies.
[00:51:05] Obviously drones are increasingly more common. And I think you’re right. I think we’re going to start to see procedures as well start to happen in homes and communities. So I think it’s a really, really interesting time.
[00:51:16] Holly Conger: [00:51:16] Hi, brain surgeries are a little further out just cause like, you know, with robotic surgery and something
[00:51:28] Dr. Nundy: [00:51:28] into your house.
[00:51:29] Holly Conger: [00:51:29] I mean, it’s more just like, you know, robotic surgery is great until something goes wrong. Like the machine breaks, you hit something and need to convert to open surgery. If the surgeon is not there. Yeah.
[00:51:40] Dr. Nundy: [00:51:40] Yeah. Yeah. Although again, I think, you know, the play, my sort of like engineering nerd counter to that is like, I think we don’t often think about the counterfactual.
[00:51:50] Like how often do surgeons make mistakes? You know, we shouldn’t be operating anymore. And, and then the other one is disparities. How many people live in a place that don’t have any surgery at all? Like up in Alaska and certainly all the places around the world I’ve worked when I was at the world bank.
[00:52:05] So you’re right. But I think this is the point of distributed. We have to think about each local context and think what is the best model starting patient first? And, you know, we may surprise ourselves. Like, it’s like when the first autonomous car crash, I was like, Oh, the car crashed. Oh my God. It’s like every day.
[00:52:25] Right?
[00:52:26] Dave Etler: [00:52:26] So it’s the same, it’s the same concept with the vaccines, you know, every time there’s a vaccine. You know, adverse reaction, that’s very serious. It ends up in the news. And so we end up thinking more about that than the fact that the vaccines are actually, you know,
[00:52:38] Dr. Nundy: [00:52:38] and
[00:52:38] Holly Conger: [00:52:38] I think it’s like, it’s all about responsibility is like, that’s the holdup is who’s responsible.
[00:52:43] If the telehealth visit, you think it’s fine. And then the patient dies from something you missed. Who’s responsible if the remote surgery goes wrong and nobody’s there to fix it, you know, like a lot of questions, it’s all about the responsibility reactive. Right? What did you as part of it, which is unfortunate, but that’s just like what I think.
[00:52:59] We’ll probably be in the way.
[00:53:01] Dave Etler: [00:53:01] So I guess my question to you doctor, before we go is you know, we’ve talked about whether doctors are ready for it.
[00:53:08] We’ve talked about whether the system is ready for it, or the patients ready for this. Are they clamoring for this or do they even know what’s possible?
[00:53:16] Dr. Nundy: [00:53:16] Yeah, I mean, I, I think so. I think that’s that cultural shift, right? That I think that. People that have had their first virtual visits, you know, have for their first home visits, you know, that have, you know, found their own vaccines, found their own tests.
[00:53:32] I think that they are realizing that a, the healthcare system it’s magnified how bad it really is and, B) it’s shown them what’s actually possible. And I think that’s unleashed something that I think will be a mega trend over the next several years. And one that I’m super excited about. Look
[00:53:51] Dave Etler: [00:53:51] forward to seeing how this all shakes out, loved the book.
[00:53:53] Thank you so much for sharing your ideas and your book with us. Care after COVID. Where can listeners find out
[00:53:59] Dr. Nundy: [00:53:59] more? Yeah, so the book’s coming out on May 4th apparently, but he can already pre-order it on your favorite online store. And and I also have a little website care after covid.org, or I’m going to a lot of the additional pieces that I write or conversations that I have we’ll, we’ll kind of be up there.
[00:54:16] And so, yeah, I would love to build community around this and just this overall change. I mean, I think, I really think it’s like that once in a century opportunity. And I think that the folks that are listening, you guys have as big a role in it or bigger than I do, given that I got a few less years ahead of me, but you know, like it’s all it’s on us.
[00:54:36] This is our moment. Well,
[00:54:38] Dave Etler: [00:54:38] thank you so much. That’s our show.
[00:54:41] Dr. Nundy: [00:54:41] Emily, Emily. Jesus,
[00:54:46] Emma Barr: [00:54:46] take me
[00:54:46] Holly Conger: [00:54:46] a minute.
[00:54:48] Dr. Nundy: [00:54:48] I
[00:54:48] Dave Etler: [00:54:48] told you
[00:54:50] Rick Gardner: [00:54:50] that was in assigned seats.
[00:54:54] Dave Etler: [00:54:54] Hey Jay, Emma, Holly, Rick. Thanks for being on the show with me today. I’m happy to be
[00:54:59] Holly Conger: [00:54:59] here.
[00:55:00] Dave Etler: [00:55:00] And what kind of Mexico intestinal fistula would I be if I didn’t. Thank you. Shortcuts for making us a part of your week. If you’re new here and you like what you heard today, subscribe to our show.
[00:55:09] Wherever fine podcasts are available. Our editors are AIG Choudhry and Eric Bozart and Alex Belzer is our marketing coordinator. The show is made possible by a generous donation by Carver college of medicine, student government. And ongoing support from the writing and humanities program. Our music is by Dr.
[00:55:24] Fox and atmosphere. Talk to you in one week.